Peripheral arteries are essential vessels that deliver oxygenated blood from the heart to the limbs and organs outside the chest and abdomen. When these arteries narrow or become blocked, blood flow is disrupted, causing pain, fatigue, and potential tissue damage. Often, this process develops silently, but it can lead to severe complications if left untreated. Knowing how peripheral arteries work is key to preventing and managing related disorders. Advances in peripheral artery disease treatment now offer multiple options to restore circulation and improve patients’ quality of life.
What is Peripheral Artery Disease?
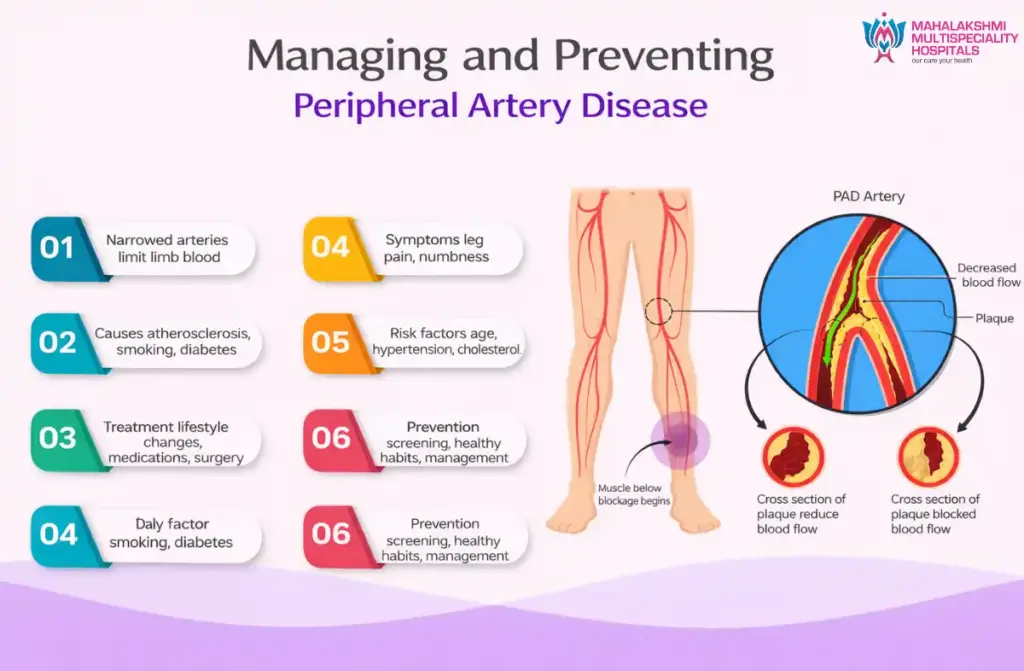
Peripheral Artery Disease (PAD) is a condition in which narrowed arteries reduce blood flow, most commonly to the legs. This restriction limits oxygen delivery to muscles and tissues, causing cramping, weakness, or numbness during activity. Understanding what is peripheral artery disease is important because it often signals widespread atherosclerosis, the buildup of fatty deposits throughout the arteries, which can affect cardiovascular health.
Symptoms of Peripheral Artery Disease
- Leg Pain and Cramping (Claudication): Muscle discomfort, tightness, or burning occurs during walking or physical activity, often easing with rest. It reflects limited blood flow to muscles under strain.
- Cold or Discolored Limbs: Legs or feet may feel colder than usual or appear pale, bluish, or darkened due to poor circulation, indicating progressive arterial narrowing.
- Slow-Healing Wounds or Ulcers: Non-healing sores on the feet or toes suggest inadequate oxygen and nutrient delivery. Without timely peripheral artery disease treatment, these wounds can become infected and risk tissue loss.
- Weak or Absent Pulse: Reduced pulse in the legs or feet is a sign of arterial obstruction and helps gauge the severity of PAD.
- Numbness, Weakness, or Hair Loss: Persistent oxygen deprivation may cause leg numbness, reduced strength, or hair thinning, emphasizing the need for early medical care.
Causes of Peripheral Artery Disease
Knowing the peripheral artery disease causes is essential for identifying individuals at higher risk and designing targeted treatment strategies.
- Atherosclerosis: Plaque buildup in arterial walls narrows vessels and can form clots that further block circulation.
- Smoking: Tobacco accelerates arterial damage by promoting inflammation and vessel constriction. Smokers are at significantly higher risk, but quitting improves circulation and response to peripheral artery disease treatment.
- Diabetes: Elevated blood sugar damages blood vessels and slows circulation, often resulting in more severe blockages and delayed wound healing.
- High Cholesterol and Hypertension: Excess cholesterol forms plaque, and high blood pressure weakens artery walls, both accelerating PAD progression.
- Genetics and Aging: Family history and natural age-related changes increase vulnerability, as older arteries are less flexible and more prone to blockages.
Risk Factors of Peripheral Artery Disease
- Smoking: Even occasional use can constrict vessels and accelerate plaque buildup.
- Diabetes: Poor blood sugar control increases the risk of severe PAD and complications.
- High Cholesterol and Blood Pressure: Both damage artery walls and expedite disease progression.
- Obesity and Inactivity: Excess weight and lack of exercise stress the circulatory system and reduce vascular resilience.
- Family History and Age: Genetic predisposition and age-related changes heighten vulnerability, making preventive care crucial.
Diagnosing Peripheral Artery Disease
Accurate detection ensures effective peripheral artery disease treatment and improved patient outcomes.
- Physical Examination and History: Doctors evaluate pulse, skin temperature, color, and risk factors such as smoking and diabetes to determine which peripheral artery disease test is appropriate.
- Ankle-Brachial Index (ABI): Compares ankle and arm blood pressures. Lower readings indicate reduced circulation and disease severity.
- Doppler Ultrasound: Measures blood flow and detects narrowed or blocked arteries to guide treatment planning.
- CT or MR Angiography: Provides detailed imaging of arteries, often used when considering surgical or minimally invasive procedures.
Stages of Peripheral Artery Disease
PAD progresses in stages, and knowing them helps guide peripheral artery disease treatment.
- Stage 1: Asymptomatic: Narrowing exists without noticeable symptoms, making screening essential for at-risk individuals.
- Stage 2: Claudication: Activity causes pain or cramping that eases with rest, indicating moderate blockage.
- Stage 3: Rest Pain: Pain occurs even at rest, often worsening when legs are elevated, showing significant circulation reduction.
- Stage 4: Critical Limb Ischemia: Non-healing wounds, ulcers, or tissue death occur due to severe oxygen deprivation, requiring urgent medical or surgical intervention.
How is Peripheral Artery Disease Treated?
The choice of peripheral artery disease treatment depends on disease stage, test results, and overall health.
- Lifestyle Changes: Quitting smoking, eating healthily, and participating in supervised exercise programs improve circulation and manage risk factors.
- Medications: Antiplatelets, statins, and blood pressure medications improve blood flow, prevent clots, and slow disease progression.
- Minimally Invasive Procedures: Angioplasty or stenting reopens narrowed arteries, restoring circulation with faster recovery.
- Surgical Options: In severe cases, bypass surgery reroutes blood around blocked arteries when peripheral artery disease test results indicate critical obstruction.
- Follow-Up Care: Regular monitoring ensures treatment effectiveness and allows early intervention for new blockages or complications.
Results of Treatment
Outcomes of peripheral artery disease treatment depend on disease stage, patient health, and adherence to lifestyle and medical recommendations.
- Improved Circulation and Reduced Pain: Restores blood flow and alleviates discomfort, increasing mobility.
- Faster Healing of Wounds: Enhanced oxygen delivery speeds recovery of ulcers and reduces infection risks.
- Better Physical Function: Patients regain endurance and independence in daily activities.
- Lower Cardiovascular Risks: Managing cholesterol, blood sugar, and blood pressure reduces heart attack and stroke risk.
- Long-Term Vascular Health: Routine monitoring maintains treatment benefits and prevents complications.
Read also: Diabetic Foot Ulcer Treatment